

Previously in this series, I’ve discussed the origins of the ketogenic diet and the biological role of ketone bodies (Part 1), if ketosis is a normal and natural state (Part 2), ketogenic diets effects on weight loss, (Part 3) whether it is good for controlling insulin resistance and diabetes (Part 4), and whether ketogenic diets can cure cancer (Part 5). Now, let’s examine the impact of the high-fat, low-carbohydrate diet on the gut microbiome and the health implications of long-term ketogenic diets.
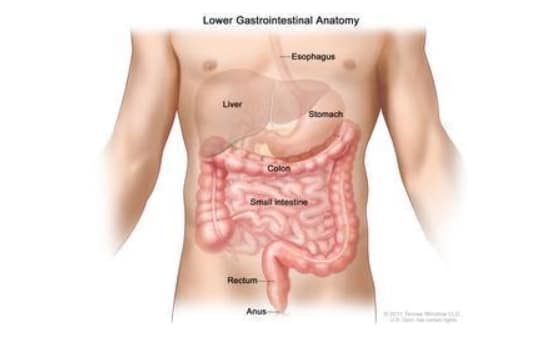
First, a short primer on the human gut and microbiome. The term gut means the entire gastrointestinal tract, from mouth to anus. The stomach harbors very few microorganisms under normal circumstances, due to its intense acidity, and the upper small intestine is also hostile due to high concentrations of bile and other digestive juices. The large intestine, however, is a different story. It provides an ideal environment for microorganisms: warm, moist, and full of food.
Our ‘microbial self’ thrives on a diverse array of carbohydrates – fiber, resistant starch and non-starch polysaccharides – found only in plants.
When we speak of the gut flora or microbiome, we’re primarily talking about the genetic material of the microorganisms that inhabit our large intestine, or colon[1]. The community of microorganisms themselves, about 100 trillion of them, is called microbiota and it is comprised of mostly bacteria but also viruses, fungi, and protozoa.[1] Their collective genome is enormous (about 3 million genes versus 23,000 genes in a human being) and it is important to us because they produce thousands of substances that can positively or negatively affect our health depending on what we feed them.
While there is no consensus on the ideal composition of the human gut microbiota, there are particular patterns of dysbiosis—underrepresentation of certain bacterial species, and overrepresentation of others—which are strongly linked with a heightened risk of various diseases. Inflammatory bowel disease, obesity, type 2 diabetes, cardiovascular disease, and cancer are just some of the diseases that have been linked to imbalanced gut microbiota[2].
The overall diversity and specific composition of our gut microbiota are affected by numerous dietary components, including total protein and proportions of protein from animal vs plant sources; total fat and proportion of saturated vs unsaturated fat; fiber; resistant starch; polyphenols; and sugar.

A high-fat diet has been found to reduce colon bacteria overall[3], while increasing total anaerobic microflora and Bacteroides counts[4]. Bacteroides are normally beneficial organisms, but overgrowth is associated with inflammatory bowel disease, severe antibiotic-resistant infections[5], and colorectal cancer[6].
The ketogenic diet is characterized by being high in fat, very low in carbohydrates, and low to moderately high in protein (depending on whether it is a classical or modified ketogenic diet—see Part 1).
A small study of people suffering from Glucose Transporter 1 Deficiency Syndrome (GLUT1 DS—a cause of epileptic seizures) found that after three months on a ketogenic diet, there was a significant increase in a group of bacteria known to produce hydrogen sulfide—a gas which causes gut inflammation and is linked to the development of inflammatory bowel disease[7].
In a study of people at high risk of metabolic syndrome, switching from a diet high in saturated fat (typical of the ketogenic diet) to a low-fat diet increased the numbers of beneficial Bifidobacterium, and this correlated with reduced fasting glucose and total cholesterol[8]—in other words, a reversal of metabolic syndrome.
A high-fat diet increases intestinal permeability—that is, it causes leaky gut, by turning off the genes that code for proteins that comprise tight junctions, the “seals” between neighboring intestinal cells[9]. Tight junctions are intended to stop unwanted or dangerous gut contents—such as undigested proteins and bacterial toxins—from leaking through the gut wall and into the bloodstream[10]. One of those toxins is endotoxin, a component of the cell walls of gram-negative bacteria. Saturated fat intake, in particular, increases the absorption of endotoxin from the gut into the bloodstream and the resulting endotoxemia triggers inflammation[11], and is associated with reduced glucose tolerance (which can eventually lead to diabetes), weight gain, and oxidative stress[12].
People suffering from major depressive disorder have been found to have higher levels of serum antibodies against endotoxin than non-depressed people, indicating leaky gut and an immune response to endotoxemia could be related to depression[13].
High fat intake also increases the amount of bile secreted by the gallbladder into the small intestine. This increases the relative abundance of bacterial species that use bile as a food source. High counts of these bacteria are associated with increased inflammation[14]. High counts of Bilophila wadsworthia have been linked to increased incidence and severity of colitis[15] and colorectal cancer and colorectal cancer[16], while Alistipes was found to be overrepresented in people suffering from major depressive disorder[17].

Proponents of ketogenic diets tend to lump all carbohydrate-containing foods together, presenting them as the root cause of the chronic diseases that plague Westernized countries.
However, when it comes to the gut microbiome, all carbohydrates are not created equal. Unrefined or minimally-processed carbohydrate-rich foods, such as whole grains, starchy vegetables, legumes, and fruits, contain non-digestible carbohydrates including fiber, resistant starch, and non-starch polysaccharides—dubbed microbiota accessible carbohydrates (MACs) by researchers.
Unlike simple starches and sugars, these non-digestible carbohydrates are not broken down by human digestive enzymes in the small intestine[18] and don’t serve as a food source for us. Instead, they make it all the way down to the large intestine where our gut microbiota ferment them, producing not only an energy source for themselves but a host of compounds that are beneficial for their hosts—us.
A diet low in MACs reduces total bacterial abundance—one of the major indicators of healthy microbiota—and the richness of their microbiome[19]. As leading gut microbiome researchers, Erica and Justin Sonnenburg put it, eating a low carbohydrate diet equates to “starving our microbial self“[20].
The consequences of this impoverishment in total numbers and diversity of gut bacteria are not yet understood, but it’s worth noting that humans who live a more ‘primitive’ hunter-gatherer lifestyle, such as the Hadza of northern Tanzania, have far greater microbial richness and biodiversity than typical Westerners—a characteristic linked to their high consumption of fibrous plant foods[21], and strongly correlated with their freedom from typical Western diseases including obesity, diabetes, and colorectal cancer.
One of the products of bacterial fermentation of MACs—specifically resistant starches and dietary fiber—is butyrate. Butyrate has an astonishingly diverse suite of benefits, including[22]:
Even ketogenic diets that are high in fiber-rich but low-carbohydrate vegetables cannot hope to achieve the quantity and diversity of MACs needed to cultivate a healthy and diverse gut microbiome. Non-fiber MACs such as resistant starch and non-starch polysaccharides are found most abundantly in whole grains, legumes, and fruits, not vegetables.
The American Gut Project—a massive citizen science project that uses “big data” to help fill in knowledge gaps about the complex links between our diet and lifestyle habits, gut microbiota, and health status—recently reported that the single greatest predictor of microbial diversity is the number of different plant foods eaten per week.[23] Participants who reported eating more than 30 different plant foods had the most diverse microbiota. It’s easy to eat this many different plant foods on a whole food, plant-based diet, but virtually impossible on a ketogenic diet that excludes most fruits, starchy vegetables, whole grains, and legumes.
Whole grain consumption is consistently linked with improved health – including decreased risk of type 2 diabetes, cardiovascular disease, and weight gain[24]–and many of the benefits of whole grain consumption are likely mediated through their effects on gut microbes.
For example, diets rich in whole grain and wheat bran are linked to an increase in the bacteria Bifidobacteria and Lactobacilli, while whole grain barley and resistant starches increase the abundance of butyrate-producing bacteria. People with advanced colorectal cancer were found to have a lower fiber intake, reduced levels of butyrate and other short-chain fatty acids, and lower counts of fiber-loving bacteria than cancer-free controls[25].

While the classic ketogenic diet contains less protein than fat, some variants are relatively heavy on protein—almost invariably animal proteins, since plant proteins come packaged with carbohydrates.
Bile-tolerant anaerobes increase with the consumption of animal-based protein[26], while the beneficial bacteria are depleted by high-protein, low-carbohydrate diets—and consequently, lower butyrate production is observed in people following such diets[27].
Fewer butyrate-producing bacteria are found in the feces of inflammatory bowel disease patients than in healthy control patients[28]. And high animal protein intake has been found to significantly increase the risk of developing this bowel disease[29].
The dysbiotic pattern of increased Bacteroides and diminished butyrate-producing bacteria has also been identified in colorectal cancer patients[30].
High-fat, low-carbohydrate ketogenic diets cause major disruptions to our microbiota, triggering leaky gut and systemic inflammation. Since the study of our microbiota is still in its infancy, the long-term consequences of the dysbiosis induced by ketogenic diets are unknown, but strong links are already evident with many chronic diseases including inflammatory bowel disease and colorectal cancer.
Our microbial self thrives on a diverse array of carbohydrates—fiber, resistant starch, and non-starch polysaccharides—found only in plants. If you want a healthy gut microbiome, and all the benefits that flow from it, the solution is simple: eat more plants.
Copyright 2024 Center for Nutrition Studies. All rights reserved.